Many people live with physical symptoms that don’t show up clearly on medical tests. Pain, fatigue, stomach problems, chest tightness, dizziness, or neurological-like symptoms may persist for months or years, even after repeated doctor visits. When tests come back “normal,” people are often told, “It’s probably stress”—a phrase that can feel dismissive and confusing.
This is where psychosomatic disorders come in.
Psychosomatic disorders are real physical conditions influenced by emotional stress, psychological factors, and nervous system responses. They are not imagined, exaggerated, or fake. The symptoms are genuine bodily experiences caused by how the brain and nervous system respond to emotional overload.
Understanding psychosomatic disorders can bring relief, clarity, and hope—especially for people who feel unheard or misunderstood.
What Is a Psychosomatic Disorder in Simple Terms?
In simple terms, a psychosomatic disorder is when emotional stress, trauma, or psychological strain causes physical symptoms in the body.
- Psycho = mind
- Somatic = body
A psychosomatic disorder happens when the mind and nervous system affect the body so strongly that physical symptoms develop, even when no clear structural disease is found.
This does not mean:
- The symptoms are imaginary
- The person is “making it up”
- The pain isn’t real
It means the body is responding to emotional or psychological stress as if it were a physical threat.
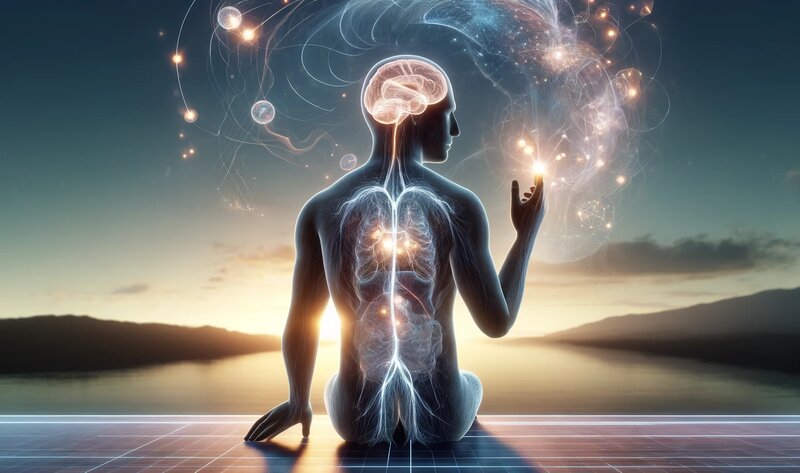
How the Mind and Body Are Connected
The mind and body are part of the same system. The brain constantly communicates with the body through:
- The nervous system
- Stress hormones (like cortisol and adrenaline)
- The immune system
- Muscle tension patterns
- Breathing and heart rate
When you experience stress, fear, or emotional pain, your body responds automatically. This response is designed to protect you. However, when stress becomes chronic or unresolved, the body can stay stuck in survival mode.
Over time, this ongoing stress response can produce real physical symptoms.
Common Symptoms of Psychosomatic Disorders
Psychosomatic symptoms vary widely and can affect almost any part of the body.
Common Physical Symptoms
- Chronic pain (neck, back, joints)
- Headaches or migraines
- Fatigue and exhaustion
- Muscle tension or weakness
- Chest pain or tightness
- Heart palpitations
- Shortness of breath
- Dizziness or lightheadedness
- Tingling or numbness
- Digestive issues (IBS, nausea, bloating)
- Skin problems (eczema, hives, itching)
- Sleep disturbances
These symptoms are often worse during stress and may improve temporarily when the person feels safe or distracted.
What Are the 7 Psychosomatic Diseases?
There is no single official list, but clinicians often recognize several common psychosomatic conditions. Below are seven frequently cited examples.
1. Tension Headaches and Migraines
Stress, emotional suppression, and muscle tension commonly contribute to chronic headaches and migraines.
2. Irritable Bowel Syndrome (IBS)
IBS is strongly linked to stress, anxiety, and trauma. The gut and brain communicate constantly, making digestion highly sensitive to emotional states.
3. Fibromyalgia
Characterized by widespread pain, fatigue, and sensitivity, fibromyalgia is associated with nervous system sensitization and stress dysregulation.
4. Chronic Pain Syndromes
Pain without clear tissue damage—such as back pain or pelvic pain—can be driven by stress-related nervous system responses.
5. Functional Neurological Symptoms
These include weakness, tremors, seizures, or numbness that resemble neurological conditions but occur without structural damage.
6. Stress-Related Skin Disorders
Eczema, psoriasis, hives, and itching often worsen during emotional stress.
7. Non-Cardiac Chest Pain
Chest pain caused by muscle tension, anxiety, or nervous system activation rather than heart disease.
What Is the Mechanism of Psychosomatic Disorder?
Psychosomatic disorders develop through a biological process, not imagination.
Step 1: Stress or Emotional Threat
The brain perceives danger—emotional, relational, or psychological.
Step 2: Nervous System Activation
The autonomic nervous system activates the fight-flight-freeze response.
Step 3: Hormonal and Physical Changes
Stress hormones increase:
- Muscle tension rises
- Breathing becomes shallow
- Digestion slows or speeds up
- Pain sensitivity increases
Step 4: Symptoms Become Persistent
If stress continues, the nervous system stays activated. The body learns this pattern and repeats it automatically, even when danger is gone.
This is why symptoms can continue long after the original stressor has passed.
Why Psychosomatic Symptoms Feel So Intense
Psychosomatic symptoms often feel more intense because the nervous system becomes hypersensitive.
This is sometimes called:
- Central sensitization
- Nervous system dysregulation
- Threat-based body response
The brain amplifies sensations to protect you, even when protection is no longer needed.
Why Medical Tests Often Show “Nothing Wrong”
Medical tests look for:
- Structural damage
- Infection
- Tumors
- Inflammation markers
Psychosomatic disorders are functional, meaning the problem lies in how systems communicate—not in damaged organs.
Normal test results do not mean symptoms aren’t real. They mean the issue is regulatory rather than structural.
Psychosomatic Disorders vs Anxiety Disorders
Psychosomatic disorders and anxiety disorders often overlap but are not the same.
- Anxiety disorders primarily affect thoughts, emotions, and fear responses
- Psychosomatic disorders primarily affect physical symptoms driven by stress
However, anxiety can worsen psychosomatic symptoms, and physical symptoms can increase anxiety—creating a cycle.
Can Psychosomatic Illness Be Cured?
Psychosomatic illness is highly treatable, and many people experience significant improvement or full recovery.
“Cure” does not always mean symptoms disappear overnight. It often means:
- The nervous system becomes regulated
- Symptoms lose intensity
- The body feels safe again
- Flare-ups become manageable or rare
The brain is adaptable. This ability to change is called neuroplasticity.
How Psychosomatic Disorders Are Treated
Effective treatment focuses on regulating the nervous system, not forcing symptoms away.
Psychological Therapies
- Cognitive Behavioral Therapy (CBT)
- Somatic therapy
- Trauma-informed therapy
- Mindfulness-based therapy
Nervous System Regulation
- Slow breathing exercises
- Gentle movement
- Grounding techniques
- Predictable routines
Emotional Processing
- Learning to feel emotions safely
- Reducing emotional suppression
- Building emotional awareness
Lifestyle Support
- Adequate sleep
- Balanced nutrition
- Reducing overstimulation
- Supportive relationships
What Makes Psychosomatic Symptoms Worse?
Symptoms often worsen with:
- Chronic stress
- Emotional suppression
- Fear of symptoms
- Hypervigilance to body sensations
- Invalidating environments
Understanding symptoms reduces fear—and fear reduction often reduces symptoms.
When to Seek Professional Help
Seek help if:
- Symptoms persist despite reassurance
- Daily functioning is affected
- Fear dominates your thoughts
- You feel emotionally overwhelmed
- You suspect unresolved trauma
Integrated care that respects both mind and body is ideal.
Reassurance: You Are Not Broken
Psychosomatic disorders are not signs of weakness. They are adaptive responses that once served a purpose.
Your body learned these responses to protect you. With safety, understanding, and support, it can learn new ones.
Healing is possible.