Introduction: Two Disorders Often Confused but Clinically Distinct
Emotional instability, impulsive behavior, and unpredictable mood changes—these symptoms can make Borderline Personality Disorder (BPD) and Bipolar Disorder seem similar at first glance. Both involve intense emotional experiences that disrupt relationships, self-image, and daily functioning. However, the root causes, patterns, and treatments of these disorders are entirely different.
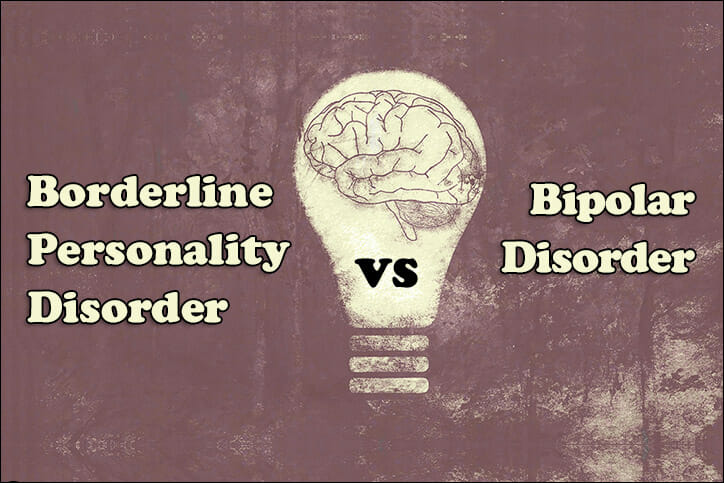
Distinguishing between BPD and bipolar disorder is essential for accurate diagnosis and effective treatment. While both fall under the umbrella of mood-related conditions in the DSM-5, bipolar disorder is primarily a mood disorder, whereas BPD is a personality disorder involving deep-seated emotional and relational difficulties.
Understanding how these conditions differ helps reduce stigma and improves empathy for those living with them.
What Is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by intense emotions, unstable relationships, and a fragile sense of identity. People with BPD often experience overwhelming feelings of emptiness, fear of abandonment, and emotional pain that can shift rapidly from one extreme to another.
According to the DSM-5, key symptoms include:
- Unstable self-image or sense of self
- Rapid emotional changes and impulsivity
- Chronic feelings of emptiness or loneliness
- Frantic efforts to avoid real or imagined abandonment
- Intense, unstable relationships that swing between idealization and devaluation
- Self-harming behaviors or suicidal thoughts in response to stress
BPD usually emerges in late adolescence or early adulthood and is often linked to early trauma, neglect, or invalidating environments. Emotional sensitivity and poor emotional regulation make it challenging for individuals to manage stress or maintain consistent behavior.
What Is Bipolar Disorder?
Bipolar Disorder is a mood disorder defined by extreme fluctuations between emotional highs (mania or hypomania) and lows (depression). These mood episodes last days, weeks, or even months, and are not typically triggered by interpersonal conflict, unlike in BPD.
The DSM-5 recognizes three main types:
- Bipolar I Disorder: Characterized by at least one manic episode that may alternate with major depressive episodes.
- Bipolar II Disorder: Involves hypomanic episodes (less intense than mania) and major depressive episodes.
- Cyclothymic Disorder: Chronic mood instability involving numerous periods of mild depression and hypomania over at least two years.
Manic symptoms may include:
- Elevated or irritable mood
- Increased energy and activity levels
- Decreased need for sleep
- Racing thoughts and rapid speech
- Impulsive or risky behaviors
Depressive episodes, by contrast, cause:
- Sadness or hopelessness
- Fatigue and loss of interest
- Sleep and appetite changes
- Difficulty concentrating
Unlike BPD, bipolar mood swings are cyclical and biologically driven, often with long periods of stability between episodes.
How to Tell the Difference Between Bipolar Disorder and Borderline Personality Disorder
While both disorders share emotional instability and impulsivity, the timing, triggers, and nature of mood shifts reveal the key differences.
Here’s how they compare:
| Feature | Borderline Personality Disorder (BPD) | Bipolar Disorder |
|---|---|---|
| Type of Disorder | Personality disorder | Mood disorder |
| Mood Changes | Sudden, short-lived (hours) and reactive to events | Long-lasting (days to weeks), often without clear trigger |
| Trigger | Interpersonal conflict, stress, fear of rejection | Biological or cyclical; not always situational |
| Self-Image | Unstable or distorted | Generally stable between episodes |
| Behavior Patterns | Impulsive, self-destructive, emotionally reactive | Manic or depressive behaviors depending on phase |
| Treatment Focus | Psychotherapy (DBT, CBT, MBT) | Medication + psychotherapy |
| Sleep Patterns | Irregular due to emotional stress | Altered during mood episodes (especially mania) |
Duration is the biggest clue.
Bipolar mood shifts last for extended periods, while BPD emotions can change multiple times a day based on interpersonal events.
For example, someone with BPD may feel rejected and spiral into despair after a friend cancels plans, whereas someone with bipolar disorder may experience a full manic or depressive episode independent of external triggers.
The Role of Sleep in Bipolar Disorder: How Much Is Enough?
Sleep is a crucial regulator of mood, especially for individuals with bipolar disorder.
During manic episodes, people often feel little or no need for sleep, yet remain highly energetic. Conversely, depressive episodes can cause excessive sleep or insomnia.
Experts recommend 7–9 hours of quality sleep each night, but consistency is even more important than duration. Irregular sleep patterns can destabilize the brain’s circadian rhythms, potentially triggering mood episodes.
Healthy sleep strategies for bipolar management include:
- Maintaining a fixed bedtime and wake time
- Avoiding caffeine or alcohol late in the day
- Creating a calming pre-sleep routine
- Using light therapy under professional supervision
- Seeking help for sleep disturbances early
By stabilizing sleep, individuals with bipolar disorder can significantly reduce relapse risk and improve emotional regulation.
Why BPD and Bipolar Disorder Are Among the Hardest Mental Illnesses to Live With
Mental health professionals often describe BPD and Bipolar Disorder as two of the most difficult psychiatric conditions due to their profound impact on relationships, daily functioning, and self-esteem.
Borderline Personality Disorder can be especially challenging because it affects one’s sense of self and stability in relationships. The intense fear of abandonment and emotional volatility can create cycles of dependency, conflict, and self-blame. Many individuals report feeling like they live on an emotional “roller coaster” they can’t control.
Bipolar Disorder, on the other hand, brings its own challenges. Manic episodes can lead to impulsive decisions, financial problems, or risky behavior, while depressive episodes can cause deep hopelessness or suicidal thoughts. The unpredictability of mood cycles often strains personal and professional life.
It’s important to note that “hardest” does not mean hopeless. Both conditions are treatable with proper care, and many people live fulfilling, stable lives once they receive accurate diagnosis and long-term support.
The Three C’s of Borderline Personality Disorder: Clinginess, Conflict, and Chaos
Mental health experts sometimes summarize the interpersonal patterns of BPD using the “Three C’s”—Clinginess, Conflict, and Chaos—to describe how the disorder manifests in relationships.
1. Clinginess
The deep fear of abandonment leads individuals with BPD to become emotionally dependent on others. Even minor signs of distance or disinterest can cause panic or desperation, resulting in clingy or demanding behavior.
2. Conflict
Relationships often feel like a constant battle. Intense emotions and misinterpretations lead to frequent arguments and breakups. This instability stems from difficulty regulating emotions and a tendency to perceive rejection where none exists.
3. Chaos
The combination of emotional swings, impulsive actions, and unstable relationships often results in chaos—both internally and externally. This chaos may manifest as self-harm, risky behaviors, or sudden shifts in life goals and values.
Recognizing the “Three C’s” helps therapists and loved ones understand that these patterns aren’t deliberate but arise from emotional dysregulation and deep-rooted insecurity.
Through therapy—especially Dialectical Behavior Therapy (DBT)—individuals can learn emotional regulation, mindfulness, and interpersonal effectiveness to reduce these cycles.
Diagnosis: How Clinicians Distinguish Between the Two
Because symptoms overlap, diagnosing BPD vs. Bipolar Disorder requires careful clinical evaluation.
Psychiatrists assess factors like:
- Duration and pattern of mood changes
- Triggering events
- Family psychiatric history
- Personality traits and coping mechanisms
Common diagnostic tools include:
- Structured Clinical Interviews (SCID-5)
- Mood Disorder Questionnaires (MDQ)
- Personality assessments for BPD features
A thorough evaluation helps prevent misdiagnosis—a common issue, as BPD is sometimes mistaken for bipolar disorder or vice versa. Mislabeling can delay effective treatment and cause frustration for patients.
Treatment and Management: Different Paths to Stability
For Bipolar Disorder
Treatment focuses on biological stabilization through:
- Mood stabilizers: Lithium, valproate, or lamotrigine
- Antipsychotics: For managing mania or mixed episodes
- Antidepressants: Used cautiously to avoid triggering mania
- Psychotherapy: Especially CBT and Interpersonal and Social Rhythm Therapy (IPSRT)
A combination of medication and lifestyle regulation (consistent sleep, stress management, and routine) yields the best results.
For Borderline Personality Disorder
Since BPD stems from emotional and interpersonal dysregulation, psychotherapy is the cornerstone of treatment:
- Dialectical Behavior Therapy (DBT): The gold-standard therapy that teaches mindfulness, distress tolerance, and emotion regulation.
- Cognitive Behavioral Therapy (CBT): Helps challenge distorted thinking patterns.
- Mentalization-Based Therapy (MBT): Builds awareness of one’s emotions and others’ perspectives.
- Schema Therapy: Addresses deep-seated negative beliefs from early life.
Medication may help manage co-occurring conditions like anxiety or depression but does not treat BPD itself.
Long-term therapy can lead to profound recovery, with many individuals eventually losing their diagnosis altogether.
Living with BPD or Bipolar Disorder: Building a Life Beyond the Diagnosis
Recovery from either condition involves more than symptom control—it’s about building emotional resilience and self-awareness.
People living with BPD or bipolar disorder can thrive by focusing on:
- Consistent therapy attendance
- Healthy sleep and daily routines
- Support groups or community connections
- Avoiding drugs or alcohol
- Practicing mindfulness and self-compassion
Both conditions benefit from a strong therapeutic alliance—trust between patient and therapist—which fosters emotional stability and hope. With commitment and support, individuals often develop greater empathy, maturity, and life satisfaction.
Conclusion: Understanding, Not Confusing
Although Borderline Personality Disorder and Bipolar Disorder share overlapping symptoms, their foundations and treatment paths are distinct.
BPD arises from deep emotional and relational struggles rooted in early experiences, while bipolar disorder stems from biological mood dysregulation.
Accurate diagnosis and compassionate treatment are key to helping individuals navigate these challenges successfully.
With proper therapy, medication (where needed), and a supportive environment, recovery is not just possible—it’s transformative.
Understanding the difference between these disorders fosters empathy, reduces stigma, and paves the way toward healing and stability for millions worldwide.