Chronic pain and depression are two health issues that affect millions of people around the world. On their own, each condition can deeply affect a person’s quality of life. But when they occur together, the challenges become even greater. Understanding the link between chronic pain and depression is important for anyone dealing with these conditions—or supporting someone who is.
In this article, we’ll explore what chronic pain and depression are, how they are connected, and what treatment options are available. Our goal is to help you feel more informed, less alone, and more hopeful about finding relief and support.
What Is Chronic Pain?
Chronic pain is pain that lasts for a long time—usually longer than 3 months. Unlike the pain from a cut or a broken bone that heals, chronic pain sticks around even after the original cause may be gone. It can be constant or come and go, and it can affect almost any part of the body.
Common Types of Chronic Pain:
- Back pain
- Arthritis (joint pain)
- Migraines or tension headaches
- Fibromyalgia (widespread muscle pain)
- Neuropathy (nerve pain)
- Chronic pelvic pain
- Pain from injuries or surgeries that never fully healed
Chronic pain doesn’t just affect the body—it affects your mood, sleep, energy, and daily life. Over time, it can wear a person down emotionally.
What Is Depression?
Depression is more than just feeling sad or having a bad day. It’s a medical condition that affects how a person feels, thinks, and functions. People with depression often feel hopeless, empty, or numb for weeks, months, or even longer.
Common Symptoms of Depression:
- Constant sadness or irritability
- Loss of interest in activities
- Fatigue or low energy
- Difficulty sleeping or sleeping too much
- Trouble concentrating
- Feelings of guilt or worthlessness
- Changes in appetite
- Thoughts of death or suicide
Like chronic pain, depression can be invisible to others—but very real to the person experiencing it.
How Are Chronic Pain and Depression Connected?
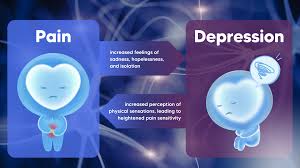
Chronic pain and depression are closely linked. In fact, studies show that people with chronic pain are 2 to 3 times more likely to suffer from depression than those without pain. And people with depression are more likely to develop chronic pain over time.
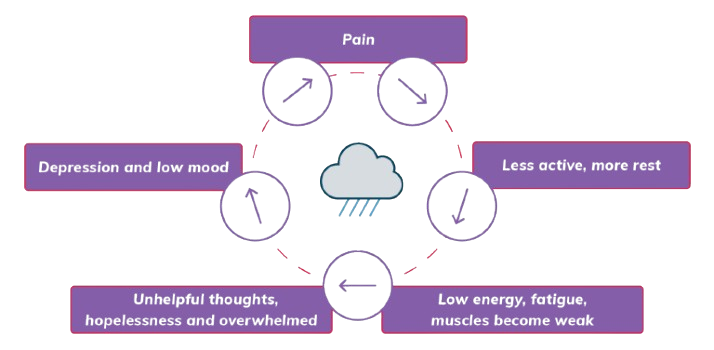
The Pain-Depression Cycle
Here’s how the cycle often works:
- Pain causes stress and frustration.
- This stress can lead to feelings of helplessness or sadness.
- These feelings can grow into depression.
- Depression can make the pain feel even worse.
- And the worse the pain feels, the more hopeless a person may become.
This cycle can feel like a trap. But understanding it is the first step toward breaking it.
Why Do They Happen Together?
There are several reasons why chronic pain and depression often go hand in hand:
1. Shared Brain Pathways
Pain and mood are both processed in parts of the brain that use similar chemicals—like serotonin and norepinephrine. If these chemicals are out of balance, both pain and mood can be affected.
2. Lifestyle Changes
When you’re in pain, you might stop doing things you enjoy, such as exercising, socializing, or working. These changes can lead to isolation and sadness, which increase the risk of depression.
3. Sleep Disruption
Chronic pain can make it hard to sleep, and poor sleep can make both pain and depression worse.
4. Stress and Inflammation
Chronic stress from living in pain can increase inflammation in the body, which may contribute to both pain and depression.
How Does This Connection Affect Daily Life?
Living with both depression and chronic pain can make daily tasks feel overwhelming. Even getting out of bed, going to work, or taking care of family can feel too hard. People may feel misunderstood, especially when others don’t “see” the pain or emotional struggle.
This combination can also strain relationships. Friends and family may not know how to help, and people dealing with these issues may withdraw or become irritable. That’s why support and understanding from loved ones—and professionals—are so important.
Treatment Options: What Can Help?
The good news is that both depression and chronic pain are treatable, and they often improve when treated together. Treatment may take time, but many people do feel better with the right support.
1. Medications
Some medications can help with both pain and mood:
- Antidepressants (like SNRIs and tricyclics) can reduce depression symptoms and ease certain types of pain.
- Pain relievers, anti-inflammatories, and nerve pain medications (like gabapentin) may also be used—but should be monitored closely by a doctor.
2. Therapy and Counseling
Mental health therapy can be extremely helpful:
- Cognitive Behavioral Therapy (CBT) helps change negative thoughts and teaches coping strategies.
- Acceptance and Commitment Therapy (ACT) helps people live with pain without letting it control their lives.
- Mindfulness-Based Stress Reduction (MBSR) can reduce stress and improve mood.
Therapists who specialize in chronic illness or pain can offer especially useful guidance.
3. Physical Therapy and Movement
Gentle physical activity—like walking, stretching, or swimming—can reduce pain and improve mood. Physical therapists can help you create a plan that works with your body.
4. Lifestyle Changes
Small daily habits can make a big difference:
- Regular sleep routines
- Balanced nutrition
- Relaxation techniques (meditation, deep breathing)
- Reducing alcohol and avoiding substance use
Even if progress is slow, these habits support both body and mind.
5. Support Groups
Talking with others who understand what you’re going through can provide comfort and practical advice. Look for chronic pain or depression support groups—online or in person.
6. Integrated Care
Some healthcare clinics offer integrated care, where doctors, therapists, and physical therapists work together on a treatment plan. This whole-person approach often leads to better outcomes.
Why It’s Important to Seek Help
If you or someone you know is struggling with chronic pain and depression, know that you’re not alone—and help is available. Too many people suffer in silence, believing their pain or sadness is something they just have to live with. But you don’t have to suffer without support.
Talk to your doctor or a mental health professional. Describe both your physical pain and how you’re feeling emotionally. The more complete the picture you give, the better they can help.
A Message of Hope
Living with chronic pain and depression can feel exhausting, lonely, and never-ending. But recovery is possible. With the right mix of treatments, support, and self-care, many people find relief—and even joy again.
You are not weak. You are not imagining things. Your pain is real, and your emotions are valid.
Healing may not happen overnight, but step by step, better days can come.