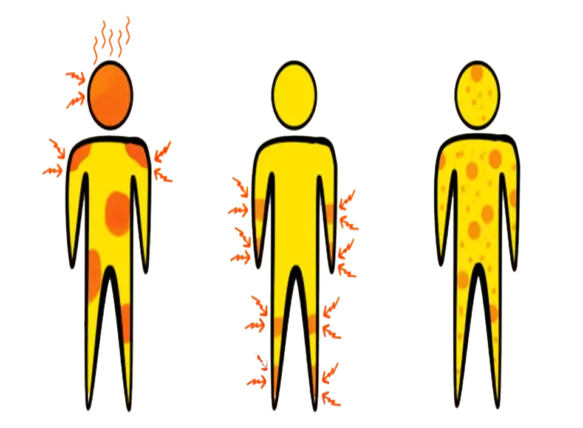
Somatization is the expression of psychological or emotional factors as physical (somatic) symptoms. For instance, some people experience headaches, nausea, back pain, chest pain, or exhaustion as a result of stress. Somatic symptom disorder (formerly known as somatization disorder) and malingering are disorders in which somatization appears.
Individuals suffering from these disorders tend to be fixated on their bodily issues. Which means they frequently seek medical guidance and care rather than psychiatric assistance.
What is somatization?
Somatization is the emergence of physical symptoms. That are ultimately caused by psychological factors and interfere with everyday functioning or cause a great deal of grief. There is no known underlying medical reason for the particular somatic complaints and symptoms. Even though the physical symptoms may or may not be connected to a medical illness.
Colorado points out that although it’s normal to have symptoms from psychological elements like stress, such a tension headache, somatization occurs when the body reacts excessively and becomes harder to control.

“Physical distress or pain can sometimes persist for a long time after a stressful or traumatic event,” the speaker states. “Non-epileptic seizures, gastrointestinal disorders, and migraines are common forms of somatization symptoms.”
Even if somatization symptoms cannot be linked to a specific medical condition. Patients are not fabricating their illnesses, she continues. “In social or professional settings, these symptoms still significantly increase stress.” Whether or whether a physical cause is uncovered, the distress people go through is real.
Somatic symptom disorder and related disorder
In somatization disorders, patients’ excessive or poorly suited thought, feeling, and behavior in reaction to the bodily issues is linked to their persistent physical symptoms. Patients frequently experience distress and struggle to carry out social, professional, or academic tasks. Among these illnesses are the following:
- Somatic symptom disorder
- Illness anxiety disorder
- Conversion disorder
- Factitious disorder
- Psychological factors affecting other medical conditions
Somatic symptom disorder
Chronic physical issues coupled with negative thoughts, feelings, and behaviors in reaction to those bodily complaints are the hallmarks of somatic symptom disorder. The symptoms are real, even though there might or might not be a corresponding medical problem. A supportive and continuous doctor-patient connection is the main emphasis of treatment. With no unnecessary treatments or tests. Doctors typically make their diagnosis based on the patient’s medical history.

Illness anxiety disorder
An individual with illness anxiety disorder is obsessed and afraid of being very sick. Once the patient has been assured there is no physical sickness and has undergone medical evaluation, the disorder is diagnosed if the worries and symptoms (if any) persist for six months or longer. Strong doctor-patient relationships are the mainstay of treatment, which may also involve the use of selective serotonin reuptake medications and behavioral therapy.
Conversion Disorder
Nervous system symptoms, such as impaired balance or coordination, limb paralysis, weakness, blindness, deafness, loss of feeling, unresponsiveness, trouble swallowing, or urine retention, are referred to as conversion disorders.
The beginning of symptoms usually happens in reaction to a stressful situation. The basis for the diagnosis is ruling out any underlying medical disease that might be the source of the symptoms. The illness is more common in women than in males, and it typically manifests in late childhood or early adulthood. Conflict in the mind can lead to the development of conversion disorder. For example, someone who disbelieves in violence but feels the want to hit someone can suddenly go numb in their arms.
Factitious disorder
In the absence of a defined motivation, this refers to the falsification of mental or physical symptoms by acting sick or self-harming. These goals could be to stay out of legal trouble, take time off from work, or collect disability benefits. In addition to fabricating symptoms, the individual might tamper with testing to convince others that they need surgery or other medical intervention. Although the person with this disease may be aware that they are fabricating symptoms, they may not understand the reason behind their behavior or may not consider it to be problematic. Although diagnosing and treating this disease can be challenging, intervention is essential to halting any major harm that the conduct may cause.
Psychological Aspects Influencing Additional Medical Disorders
This is identified when behavioral or mental health issues worsen the course of a pre-existing medical condition, including diabetes or heart disease, raising the possibility of suffering, passing away, becoming disabled, or needing hospitalization. These reasons can include refusing to get tested, not following through on treatments, or downplaying the importance or severity of symptoms. Treatment failure and the aggravation of preexisting medical issues are characteristics of this illness. Patient education and psychotherapy are examples of intervention techniques.
Malingering
To distinguish it from factitious disorder, this is the deliberate fabrication of psychological or physical symptoms in the presence of a benefit, such as obtaining substances of abuse, receiving time off from work, or evading military service. Because the traditional model of patient care is predicated on a doctor-patient connection that presumes patients are being sincere, this condition is difficult for doctors to handle. Because of this, physicians may be reluctant to check for malingering in a patient.
Malingering is diagnosed only when no medical condition can be ruled out. Following a careful assessment of the patient’s psychological state, medical history, and relevant laboratory tests.
Causes of Somatization Symptom and Related Disorders
Although the origins of somatization symptom disorders can vary, prior events and stresses are frequently the root cause of somatization symptom disorders and related diseases, according to Dr. Schwartz. “These health effects can be partially attributed to dysautonomia, which is a fancy term for the dysregulation of the autonomic nervous system (ANS), which can be brought on by prolonged stress and unresolved post-traumatic stress.”
According to a 2019 Frontiers of Psychology article, somatization symptoms can co-occur with a variety of mental illnesses. such as
- a close correlation between symptoms of anxiety and depression.
- A moderate correlation with manic and schizophrenia symptoms.
- Weak correlation between antisocial personality traits and signs of substance abuse.
Treatment for Somatization Symptom and Related Disorders
The precise diagnosis determines the course of treatment for somatization symptom disorders. For instance, factitious disorder and sickness anxiety disorder have different treatment needs. Treatment for somatization symptom disorder usually entails consultations with both a psychiatrist or psychologist. And a general practitioner or other medical provider (which is partly responsible for the increased medical expenditures mentioned above).
Raja Selvam, PhD., a licensed clinical psychologist and the creator of the therapy modality Integral Somatic Psychology. states that “usually, after medical tests do not reveal a medical cause, a psychiatrist or psychologist or another mental health professional will diagnose the person’s persistent physical symptom as a possible symptom of somatization.” When a client sees a mental health professional, the therapist will use the therapeutic modality with which they are trained.
According to a 2016 American Family Physician article, medical professionals should treat SSD patients with the following:
- Making short-term, routine appointments to prevent the requirement for symptoms in order to make an appointment
- forming a therapeutic alliance that is cooperative with the patient
- recognizing and validating symptoms after a patient’s evaluation for other physical and mental health conditions
- Reducing the amount of diagnostic testing
- reassuring the patient that there are no longer any major medical conditions
- teaching people how to manage their bodily symptoms
- Choosing functional improvement as the therapeutic objective as opposed to cure
- Referring patients to sub specialists and mental health providers in a suitable manner