Depression that develops after childbirth is known as postpartum depression (PPD). Not simply the individual giving birth is affected by postpartum depression. Adoptive parents and surrogates may also be impacted. After having a child, people go through hormonal, physical, emotional, economical, and social changes. Postpartum depression symptoms may be brought on by these changes.
Know that you are not alone in experiencing postpartum depression, that it is not your fault, and that there is support available. Your medical professional can help you feel better by managing your symptoms.
Postpartum depression
Many women have postpartum depression, or PPD, which is a medical illness that follows childbirth. Strong depressive, anxious, and fatigued symptoms that persist for a long period after giving birth. You may also find it difficult to care for both yourself and your child as a result of these emotions. PPD may manifest at any point following childbirth. Usually, it begins one to three weeks after giving birth. To become better, it needs to be treated.

One type of prenatal depression is PPD. This type of depression strikes either during or during the first year following childbirth. PPD is the most frequent issue that newlywed mothers face. Up to 1 in 7 women (about 15%) may be affected.
Types of Postpartum depression
There are three types of postpartum depression.
Baby blues or postpartum blues
After giving birth, 50% to 75% of people experience the baby blues. You will frequently cry for extended periods of time without any apparent cause if you’re having the baby blues, along with feelings of melancholy and anxiety. Usually, the illness starts one to four days or within the first week following delivery. Even though it hurts, if care is not received, the ailment normally goes away in two weeks. Also Seeking support and assistance from friends, family, or your partner is the best course of action.
Postpartum depression
About 1 in 7 new parents experience postpartum depression, a far more dangerous disorder than the baby blues. Pregnancy increases your chances of postpartum depression by 30% if you have experienced it previously. You might feel guilty, anxious, and also incapable of taking care of yourself or your child. You might also cry a lot, experience highs and lows in intensity, and be easily agitated and exhausted. Mild to severe symptoms may start a week after delivery or develop progressively over the course of up to a year. Antidepressants and psychotherapy are very effective forms of treatment, although symptoms can linger for several months.
Postpartum psychosis
Emergency medical intervention is necessary for postpartum psychosis, a severe form of postpartum depression. Just 1 in 1,000 people will have this very uncommon illness after delivery. Usually starting shortly after delivery, the symptoms are intense and persist anywhere from a few weeks to several months. Severe agitation, disorientation, depression, guilt, insomnia, paranoia, delusions, hallucinations, hyperactivity, fast speech, or manic episodes are among the symptoms. Because postpartum psychosis increases the risk of suicide and injury to the unborn child, it needs to be treated medically very away. Medication, psychotherapy, and hospitalization are typical forms of treatment.
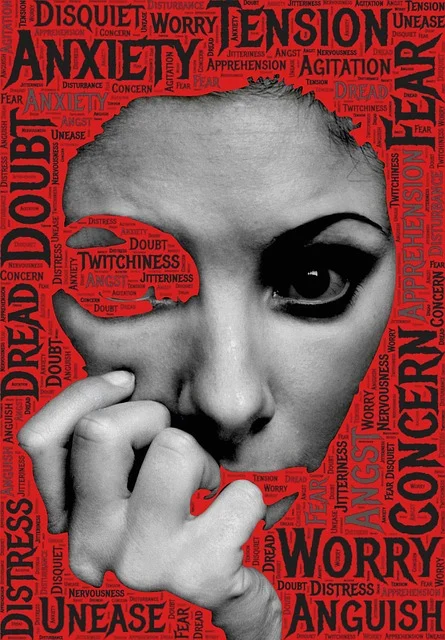
Symptoms of postpartum depression
Some people believe they are bad parents for feeling the way they do, or they feel guilty about their symptoms. Depression following childbirth is very prevalent. Also It doesn’t make you a bad person—you’re not the only one who feels this way.

Some symptoms of postpartum depression include the following:
- Feeling depressed, remorseful, hopeless, or unworthy.
- Feeling tense or too concerned.
- Loss of interest in past interests or pastimes.
- Appetite swings or abstinence from eating.
- Reduction in drive and vigor.
- Having trouble falling asleep or always wanting to sleep.
- Crying excessively or without cause.
- Difficulty concentrating or thinking.
- Suicidal thoughts or the desire to pass away.
- Anxiety around your infant or a lack of interest in them.
Causes of postpartum depression
The specific cause of PPD is unknown. Any woman can experience it after giving birth. Among the potential reasons are:
Genes
The components of your body’s cells called genes contain the instructions necessary for your body to develop and function. Parents pass on their genes to their offspring. People who have depressed family members tend to experience depression more frequently. This is referred to as a depressed family history.
After pregnancy, hormone levels change.
In your body, hormones are substances. Some aid in mood and emotion regulation. Your body produces more progesterone and estrogen when you are pregnant. But these hormones immediately return to normal within the first 24 hours of giving delivery. PPD might result from this abrupt decrease in hormone levels.
Low level of hormones
Hormone levels in the thyroid. The thyroid gland, located in the neck, aids in the body’s utilization and storage of food-based energy.

Risks factors
Postpartum depression may strike every new mother, and it doesn’t have to be the first kid to arrive. On the other hand, your risk rises if:
You’ve experienced depression in the past, either before or after becoming pregnant.
- Bipolar disorder is what you have.
- You had a prior pregnancy and experienced postpartum depression.
- Family members of yours have experienced depression or other mood disorders.
- You’ve gone through difficult experiences in the last year, such illness, job loss, or troubled pregnancy.
- Your baby need special care or has other health issues.
- You’ve had several births, such as twins or triplets.
- You have trouble nursing.
- You and your husband or partner are experiencing difficulties in your relationship.
- Your network of support is inadequate.
- You’re having money issues.
- The unintended pregnancy occurred or unwanted.
Prevention’s
Inform your healthcare practitioner as soon as you learn you are pregnant or if you want to get pregnant if you have a history of depression, particularly postpartum depression.
During pregnancy
Your healthcare practitioner can keep a close eye out for any signs of depression during your pregnancy. A depression screening questionnaire is available for you to fill out both before and after you give birth. Support groups, psychotherapy, and other therapies can occasionally be used to address minor depression. Antidepressants might be advised in different circumstances, including while pregnant.
After your baby is born
Your doctor might advise an early postpartum examination to look for signs of postpartum depression after your baby is born. Treatment can start sooner the earlier it is discovered. If you’ve already experienced postpartum depression, your doctor could advise talk therapy or also can have antidepressant medication right away.
Treatment
Treatment for postpartum depression varies based on the kind and intensity of symptoms. Anti-anxiety or antidepressant medications, talk therapy or cognitive behavioral therapy, and also involvement in support groups are among the available treatment options.

Medication for depression, anxiety, and psychosis may be part of the treatment for postpartum psychosis. Until you reach stability, you can also be admitted to a treatment facility for a few days. In the event that this treatment is ineffective, electroconvulsive therapy, or ECT, may be useful.
Don’t think that nursing prevents you from taking medication for anxiety, sadness, or even psychosis. Discuss your alternatives with your healthcare professional.



Pingback: Epilepsy/ seizures : causes, symptoms & treatment -