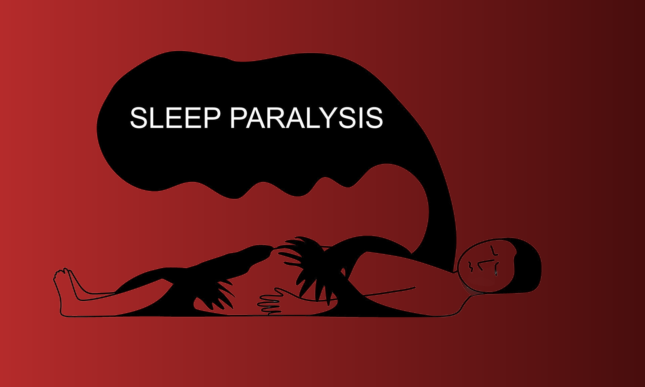
The inability to move just before going to sleep or waking up is known as sleep paralysis. It’s only momentary. Your brain facilitates the relaxation of your arm and leg muscles as you sleep. You’re trapped in between sleep stages if you have sleep paralysis. By identifying the cause of your symptoms and taking appropriate action, you can prevent more episodes.
This articles explains sign and symptoms, all possible causes, diagnostic criteria and treatment.
Sleep paralysis
When you are unable to move any part of your body just before going to sleep or when you wake up, it is known as sleep paralysis. It takes place when your body is transitioning from a sleep-wake state. An episode is brief, lasting anywhere from a few seconds to a few minutes. This kind of Parasomnia exists.
During a bout of sleep paralysis, you’ll probably experience fear or anxiety. You might have confusion when it’s over because you’ll be able to move your body normally again. You can develop anxiety about falling asleep after just one episode of sleep paralysis. This may have an impact on your day-to-day mood and functioning. When you’re experiencing an episode of sleep paralysis, there’s no cure accessible.
Signs and symptoms
Sleep paralysis is not a life-threatening condition. Having knowledge of the symptoms might ease anxiety. The inability to move or talk is the most typical sign of a sleep paralysis episode. A typical episode lasts anywhere from a few seconds to two minutes.
You might additionally encounter:
- sensations such as being pushed down
- perceptions of someone or something being in the room
- panic
- Hypnagogic and hypnopompic experiences (HHEs), which are defined as hallucinations that occur during, just before, or after sleep.
Additional signs and symptoms could be:

- breathing problems and
- a sense of impending death
- Perspiration
- aching muscles
- headaches
- apprehension
Usually, an episode ends on its own, or when you are touched or moved by someone else. During an episode, you might be conscious of what’s going on, yet you still can’t move or speak. After the temporary paralysis goes away, you might also be able to remember the specifics of what happened.
A small percentage of people occasionally have dreamy hallucinations that can be frightening or unsettling, but they are not dangerous.
Causes of sleep paralysis
It’s unclear exactly why or how it occurs. Because sleep paralysis typically occurs as a person is entering or exiting REM sleep, researchers think that disruptions in the rapid eye movement (REM) cycle are the source of the condition. Your muscles are usually paralyzed by your brain at that point, preventing them from acting out your dreams. However, during sleep paralysis, your consciousness is somewhat conscious, meaning you are aware that you are immobile.
It is uncertain what specifically causes sleep paralysis. Medical professionals observe that they may occur with the following:
- Narcolepsy.
- Insufficient sleep (sleep deprivation).
- Erratic sleep patterns, also known as shift work sleep disorder.
- Apnea obstructive sleep.
- Mental health issues such as panic disorder, anxiety, bipolar disorder, or post-traumatic stress disorder (PTSD).
- Some drugs (such as those used to treat ADHD).
- Addiction to substances (SUD).
Diagnosis of sleep paralysis
Following a physical examination and a sleep assessment, medical professionals either confirm or rule out sleep paralysis. What your provider might inquire about:
- Your symptoms, including the frequency, type, and timing of your sleep paralysis episodes.
- The amount and caliber of sleep you receive, including the number of hours you spend asleep at night and if you experience daytime fatigue.
- Your medical background, including the medications you now use and any history of alcoholism, drug use, or smoking.
- Also Your mental state, including whether you’re under stress or whether you suffer from an underlying mental illness like depression or anxiety.
- Your family’s medical history and whether you know of any biological relatives that suffer from sleep paralysis.
If your doctor believes you have a sleep disorder such as narcolepsy, which results in sleep paralysis, they may suggest testing. You might require:

- A polysomnogram: A polysomnogram, often known as an overnight sleep study, tracks your heart rate, respiration, and mental activity as you sleep. It might make it possible for medical professionals to see a paralysis episode or identify conditions like sleep apnea.
- Multiple Sleep Latency Test (MSLT): The Multiple Sleep Latency Test (MSLT) gauges the type of sleep you get during a nap as well as how quickly you fall asleep. The exam assists in identifying conditions like narcolepsy.
Treatment
Overall, the best way to treat sleep paralysis is not well supported by scientific research. Many feel guilty following bouts because they don’t know that the ailment is really prevalent. Thus, it can be helpful if a doctor acknowledges and normalizes their symptoms.
Improving sleep hygiene is a popular goal in preventing sleep paralysis because of the link between sleep paralysis and other sleeping issues. Consulting a physician is a first step towards treating sleep paralysis, as it allows for the identification and treatment of underlying issues that may be aggravating the frequency or intensity of episodes.

A better night’s sleep and more regular sleep are possible with the help of certain sleep hygiene practices.
- Create a routine: Even on the weekends, stick to the same timetable for going to bed and waking up. You can become more at ease and relaxed by following a calming pre-bedtime ritual.
- Make the most of your sleeping area: Choose the ideal mattress and pillow for your needs while furnishing your bed. Designing your bedroom with minimal light or noise intrusion is also beneficial.
- Reduce the use of drugs: Limit your intake of caffeine and alcohol, especially at night.
- Eliminate distractions: Before going to bed, put electronics—including cellphones—away for at least an hour.
Cognitive behavioral therapy for insomnia (CBT-I) is a talk therapy that aims to reframe negative thoughts and emotions that interfere with sleep, and it often includes improving sleep hygiene. CBT has a proven history of success. When dealing with mental health issues, view the source. There is a particular type of CBT designed for treating sleep paralysis.
How to prevent sleep paralysis
A few easy changes to your lifestyle can help reduce symptoms or the frequency of episodes. Some of these include:
- Decrease the amount of stress in your life.
- Regular exercise should be done away from nighttime.
- Get enough sleep.
- Keep a consistent sleep routine.
- Make a note of all the medications you take for any ailments.
- To prevent possible adverse effects, such as sleep paralysis, be aware of the interactions and side effects of the many medications you are taking.
- Steer clear of sleeping on your back by switching to your side.
These suggestions may also aid in avoiding sleep paralysis:
- counseling for trauma in therapy
- Breathing techniques
- Yoga might help you recover your sense of agency over your body.
If you suffer from worry or depression, for example, taking an antidepressant may help reduce instances of sleep paralysis. Antidepressants can diminish sleep paralysis by assisting in the reduction of dream frequency.